Following are tools created by the author of The Vermont Mask Survey to help people understand the science behind the guidance.

What is the evidence that wearing masks in the community setting is Beneficial?
According to the World Health Organization’s December, 2020 publication titled Guidance on Mask Use in Community Settings (page 8):
“At present there is only limited and inconsistent scientific evidence to support the effectiveness of masking of healthy people in the community to prevent infection with respiratory viruses, including SARS-CoV-2.”
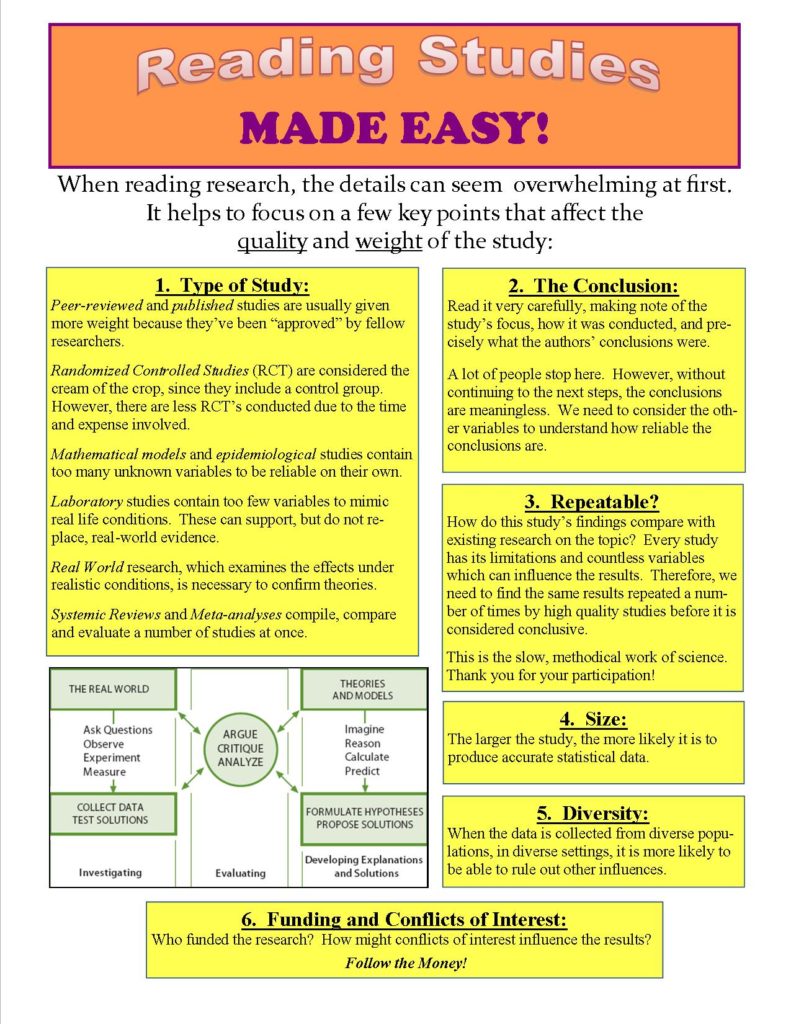
Every statement should be supported by research:
The Centers for Disease Control (CDC) provide references to support their conclusion that masks are safe and effective. The list of references looks impressive, but do the studies referenced actually support their conclusion? To find out, we need to learn how to read and evaluate the research for ourselves.
Readers may be wondering why the “restaurant study” and the “choir study” we heard so much about in the spring of 2020 are not included on the CDC’s reference list. Despite the media’s fascination with these stories, these examples did not provide evidence that infections were caused by talking or singing with others (though many people were convinced by them).
Some of the obvious flaws in the “Restaurant” and “Choir” examples include:
- being retrospective examinations (after-the-fact), it is impossible to do a true “study” of the events;
- these singular events cannot be repeated;
- participants shared surface contacts and ate food together (more likely causes of infection than talking or singing);
- suspected “spreaders” were symptomatic (coughing), therefore the results have no relevance to people without symptoms; and
- participants may have been infected by another source.
Is Amy Misleading Us? Follow the links below to read the research she is referring to, and learn about the people behind its publication: Study Quoted by Amy Goodman: https://www.medrxiv.org/content/10.1101/2020.05.27.20115139v6 MedRxiv on Youtube: https://www.youtube.com/watch?v=ChhCC1EsSzE
What Evidence Does the CDC Provide Regarding the SAFETY of Masks?
First, a word about Blood Oxygen Levels:
While several of the studies listed by the CDC refer to the fact that blood oxygen levels do not drop when wearing a mask, it is well understood that measurement of blood oxygen levels is not an appropriate way to assess oxygen deprivation.
Our blood oxygen levels (saturation) do not usually change, even when we engage in physical activity which requires increased exchanges of those gases in order to fuel our muscles. Therefore, OSHA and the CDC recommend that supervisors of respiratory protection pay close attention to other symptoms, such as difficulty breathing, headaches, and rising CO2 levels. (See OSHA’s A Guide to Industrial Respiratory Protection and CDC’s NIOSH page for more details.)
In May of 2021, the CDC added 9 additional references to their “Scientific Brief” to support their assertion that masks cause no “significant adverse health effects.”
Below is a summary of what the CDC’s references have to say regarding the safety of masks:
From the CDC’s “Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2”:
| CDC Reference and Link: | Findings Not Relevant to Safety of Prolonged Community Use Because… |
| 57. The effects of wearing facemasks on oxygenation and ventilation at rest and during physical activity. https://pubmed.ncbi.nlm.nih.gov/33626065/ | Measures Blood-Oxygen Levels after 10 minutes of use |
| 58. Peripheral Oxygen Saturation in Older Persons Wearing Nonmedical Face Masks in Community Settings. https://jamanetwork.com/journals/jama/fullarticle/2772655 | Measures Blood-Oxygen Levels Conflict of Interest Disclosures: Dr Chan reported receiving a speaker’s fee from Bayer outside of the submitted work. |
| 59. Effect of Face Masks on Gas Exchange in Healthy Persons and Patients with Chronic Obstructive Pulmonary Disease. https://pubmed.ncbi.nlm.nih.gov/33003954/ | Measures Blood-Oxygen Levels Is a letter to the editor- not a study |
| 60. “You can leave your mask on”: effects on cardiopulmonary parameters of different airway protection masks at rest and during maximal exercise. https://erj.ersjournals.com/content/early/2021/02/04/13993003.04473-2020 | 12 Healthy Adults. Article does not provide the length of time being studied. Conclusions: “Protection masks are associated with significant but modest worsening of spirometry and cardiorespiratory parameters at rest and peak exercise. The effect is driven by a ventilation reduction due to an increased airflow resistance.” Full text is unavailable to the public. |
| 61. Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. https://pubmed.ncbi.nlm.nih.gov/22326638/ | 1 hour of use in 20 subjects found: increased CO2 measurements, increased heart and respiratory rate, decreased skin temperature on face around the mask, increased temp’s on skin under the mask. Full text is unavailable to the public. |
| 62. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7646657/ | 16 healthy, non-smoking, athletic males. “In conclusion, in healthy subjects, short-term moderate-strenuous aerobic physical activity with a mask is feasible, safe, and associated with only minor changes in physiological parameters, particularly a mild increase in EtCO2. [EtCO2 tracks respiratory rate as well as a breath-by-breath trend of CO2 as it is eliminated from the lungs.] Subjects suffering from lung diseases should have a cautious evaluation before attempting physical activity with any mask.” Discussion: “The increase in EtCO2 may be explained by the fact that re‐breathing of the expired air which remains within the mask practically increases the dead space and may contribute to a mild hypercapnia…. Acute respiratory acidosis can cause headache, confusion, anxiety, decreased exercise tolerance, and at extreme levels, dim vision, vomiting, disorientation, hemodynamic instability, drowsiness, and stupor (CO2 narcosis). Prolonged exposure to mildly increased levels of CO2 is commonly referred to as “sick building syndrome” and may cause headache, fatigue, difficulty concentrating, and increase in HR and BP.” |
| 63. Face Masks and the Cardiorespiratory Response to Physical Activity in Health and Disease. https://pubmed.ncbi.nlm.nih.gov/33196294/ | Data from models of other devices. Measuring blood oxygen levels. Confirms subjects experience symptoms of oxygen deprivation and CO2 elevation (difficulty breathing and fatigue). Explains physiology and why lab models of other devices are not applicable to prolonged community use of cloth face masks: “The discrepancy between studies on face masks and studies adding external resistance to a breathing apparatus may be related, at least in part, to the type of resistance used… moisture- and temperature-related factors with face masks versus mouthpieces, and flexibility of soft face masks that may collapse and potentially increase dyspnea during exercise.” (p. 6) FOUND THAT FOR OLDER ADULTS: “There is a need for further data on the effects of face masks on the cardiopulmonary response to exercise in this population.” (p. 6) PEDIATRICS: “There are important differences in respiratory physiology in infants and young children as compared with adults (see Reference 55 for review). Infants and young children have underdeveloped accessory muscles of respiration and thus rely more on the diaphragm for most of the Wb. An increase in respiratory muscle work is largely accomplished by an increase in the respiratory rate, and the diaphragm can become fatigued more quickly than in adults. Children under the age of 6 years have proportionally more extrathoracic anatomical dead space owing to the larger ratio of head size to body size (56). These anatomical differences combined with an inherently higher basal metabolic rate place infants and young children at greater risk of respiratory failure than adults from various significant health threats. These differences decrease as children age, and other than in children younger than 2 years and those with significant respiratory or neurological conditions, there are no significant differences in respiratory physiology for older children and adolescents that are expected to substantially alter the effects of masks as described above, but additional data are needed to clarify this issue.” SEX BASED DIFFERENCES: “Compared with males, females have smaller lungs and rib cages and disproportionally smaller large conducting airways (57).” PATIENTS WITH CARDIOPULMONARY DISEASE: “On the surface, the addition of a small increase in the Wb and reinspiration of low concentrations of CO2 with any type of face mask would appear to pose more problems for individuals with underlying cardiopulmonary disease. Other drawbacks for such individuals with face-mask wearing may include anxiety and greater dyspnea, reduced fine-motor performance, possible cognitive effects as a result of slight CO2 retention and mildly increased hypoxemia, and increased Wb. Concludes: “…for some individuals with severe cardiopulmonary disease, any added resistance and/or minor changes in blood gases may evoke considerably more dyspnea and, thus, affect exercise capacity.” |
| 64. Assessment of Respiratory Function in Infants and Young Children Wearing Face Masks During the COVID-19 Pandemic. https://www.sciencedirect.com/science/article/abs/pii/S0761842517309415?via%3Dihub | Only studied effects for 30 minutes. Found that walking for 30 minutes caused significant increases in respiration and pulse rate, and almost a ¼ drop in pulse strength. |
| 65. Effect of a surgical mask on six minute walking distance. https://www.sciencedirect.com/science/article/abs/pii/S0761842517309415?via%3Dihub | 44 Healthy Subjects. 6 minutes, walking. Concludes: “Dyspnea variation was significantly higher with surgical mask (+5.6 vs. +4.6; P < 0.001) and the difference was clinically relevant.” [Dyspnea means difficulty breathing.] Full text is unavailable to the public. |
Below are a few reasons why the latest CDC report (published 3/5/21) is “inconclusive“:
1. Peer-Reviewed? Peer-review by objective professionals in the field helps assure that the study used reliable data and means, resulting in accurate conclusions. Are studies published by the CDC peer-reviewed?
This study was published as an “Early Release” in the CDC’s Morbidity and Mortality Weekly Report (MMWR). Studies in the MMWR are peer-reviewed by CDC staff in order to be sure that they conform with CDC policy. The contents are reviewed to be sure they conform with policy, not the other way around:
“Although most articles that appear in MMWR are not ‘peer-reviewed’ in the way that submissions to medical journals are, to ensure that the content of MMWR comports with CDC policy, every submission to MMWR undergoes a rigorous multilevel [internal] clearance process before publication.
“By the time a report appears in MMWR, it reflects, or is consistent with, CDC policy.”
Page 4, https://www.cdc.gov/mmwr/preview/mmwrhtml/su6004a2.htm
If this is the case, then how does the CDC adjust their policy so that it aligns with emerging scientific evidence?
2. Mathematical Model: The study’s conclusion is not based on real-world events, but on statistics run through a mathematical model. Models are never able to include all of the real-world factors that are involved. The accuracy of models rely on the weight given to each factor in the equation, and this is impossible to asses when there is no real-world data to use as a baseline. Also, the reliability of the results depends on the reliability of the data being used.
For example, are the numbers used in the model accurate? What are the definitions of a COVID-19 “case” and a “death”? Did each county use the same definitions?
To check how accurate these numbers are, see the CDC definitions of a “case” and a “death”: https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/
3. Population-Level Statistics: This study used county-level data from U.S. counties where mask mandates were implemented. While studies of populations, also called “epidemiological” studies, can be informative, they are not conclusive on their own. This is because each population is influenced by many factors which are impossible to adjust for accurately, such as age, environment, habits, economics, etc…
Was compliance with the mandate equal among each county’s population? How did the average age, hygiene habits, or work environments of each population effect each result?
There are countless factors to consider in the real-world. This is why studies of other populations find conflicting results. For example, Rational Ground compared statewide data and found that mask mandates had no effect. To see the charts, go to their website: https://rationalground.com/post-thanksgiving-mask-charts-still-no-evidence-that-masks-work/
4. Correlation Does Not Equal Causation: Just because two things happen at the same time, that does not mean that one caused the other.
There are countless factors to consider in order to determine what caused the effect, especially when studying entire populations. It’s impossible to rule out all the other influences in one study. That is why the most conclusive results are those that can be repeated again and again, showing the same results in different situations, have a control group which does not have the intervention so that a fair comparison can be made, and are double-blind (hiding the control-group) so that the researchers’ bias cannot influence the results.
To this day, there are no repeatable, double-blind, or controlled studies demonstrating benefits of masks in the community setting.
In fact, the only randomized-control study on the subject of cloth masks found that health care providers who wore them were MORE likely to spread the flu: A cluster randomised trial of cloth masks compared with medical masks in healthcare workers | BMJ Open
5. Mask Wearing in Combination with Other Strategies: During the study period, the people in those counties were also asked to use other measures to reduce the spread of the virus, including travel restrictions, shut-downs, social distancing, hand-washing, etc… Therefore the effects of masks alone is unclear.
Until we know the effects of masks alone, we cannot accurately estimate their affect compared with the other measures.
6. Selective Time Frame: The CDC study only looks at the first 100 days after mask mandates were implemented in select counties. Since most mandates were implemented in the spring and summer, when the number of flu cases naturally drops, we would expect a natural decrease in cases during this period. What happened after the first 100 days? Numbers went up again in the fall in every state.
In order to assess if masks made a difference, we would need to look at the numbers in the fall and compare them with states that did not have mandates. (See the Rational Ground research cited in #3 above.)
7. Significant Difference? Is 1.8% drop in cases after 100 days a statistically-significant number? Or, is it too small to be considered accurate? In the first 20 days, there was only a .5% and .7% decrease. This number came from averaging a large number of U.S. counties, so it is actually a broad average.
This is the best result the CDC has been able to demonstrate so far, after one year of mandates. Is this number large enough to “prove” that the effort is making a difference?

8. Cost/Benefit Analysis: If about 300 million people live in the U.S., and the country has had about 560,000 deaths, then people in the U.S. have about a 1 in 535 chance of becoming a COVID-19 “death.” If this CDC study is accurate, then 100 days of masks mandates may decrease each person’s chance by about 1.9%, bringing the risk down to about 1 in 525.
In exchange for that reduction, what percentage of the population is being harmed?
Public officials, business owners, and schools have been asking the general population to wear masks for a year now. To this day, there are no studies demonstrating the safety of using masks in the community setting, as they are currently only authorized by the FDA for emergency use.
Meanwhile, we have growing evidence of some of the immediate harms people are suffering from wearing masks (see the Vermont Mask Survey Final Report for a full discussion of the harms). Most of the costs will be seen decades in the future, and are difficult to assess accurately right now.
Stanford University’s Baruch Vainshelboim published a Health Hypothesis this winter which clearly outlines the various types of physical, mental, and social harms the general population is risking with the mask mandates.
When the lack of evidence of benefit is considered against the potential for added years of disability faced by every person living under the mask mandates, the urgent need for debate becomes apparent.
Below are a few slides demonstrating some of the points above:
Here’s an Example:
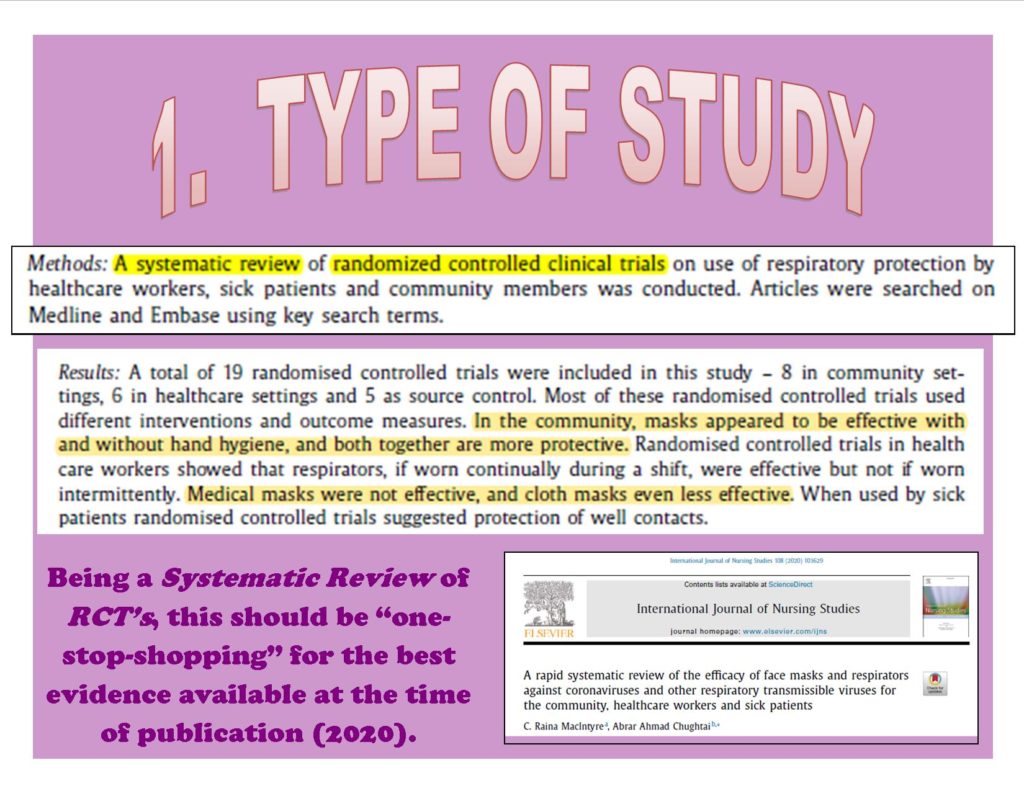
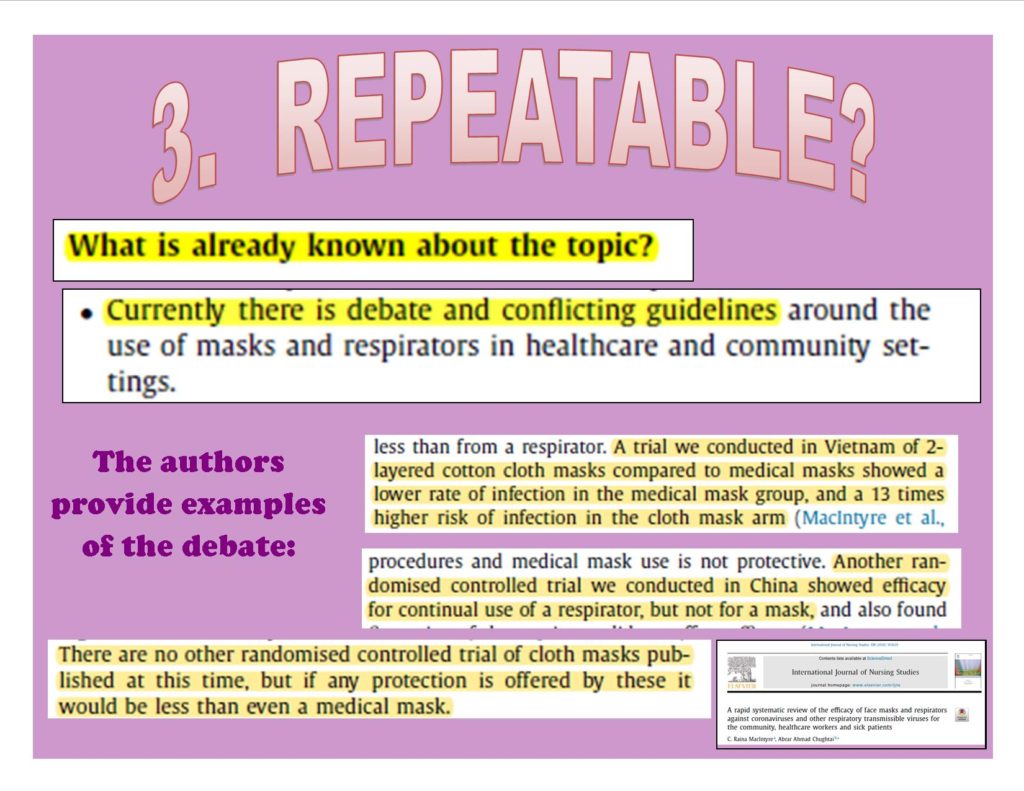
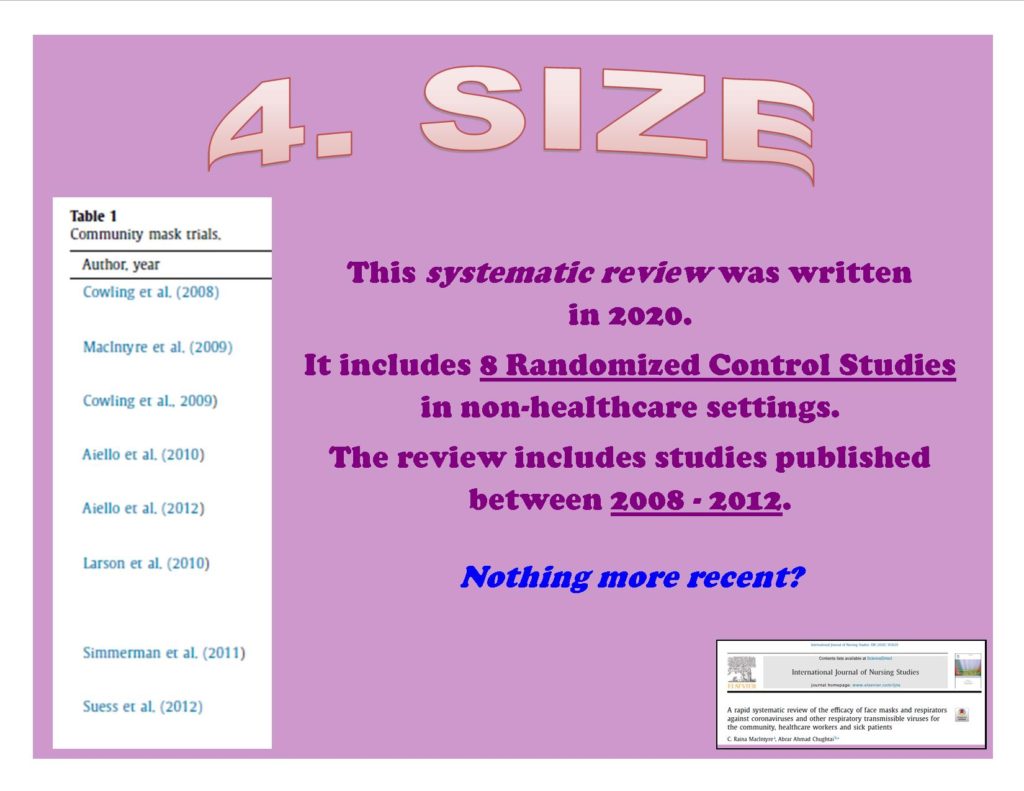
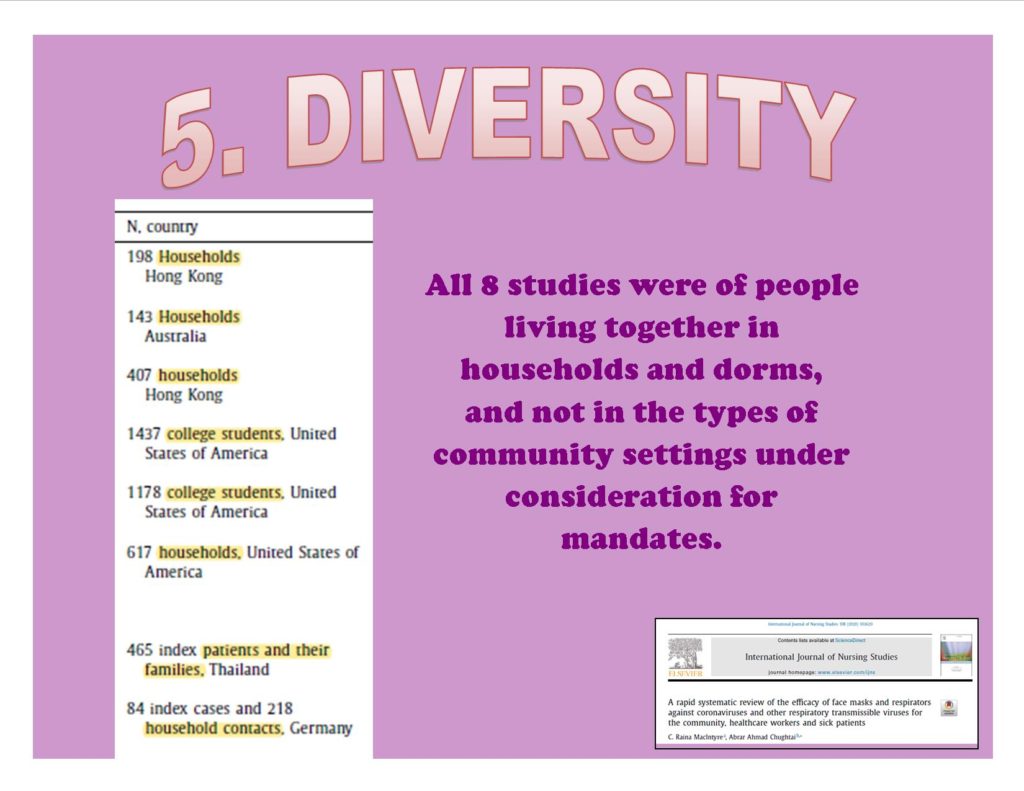
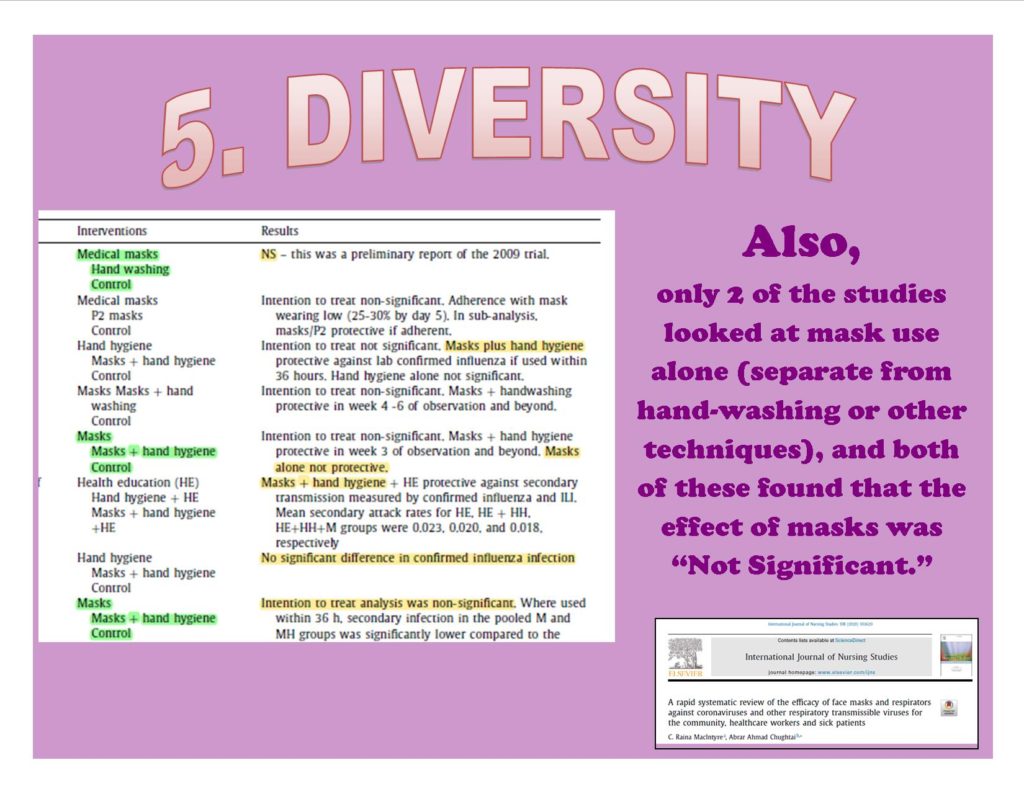
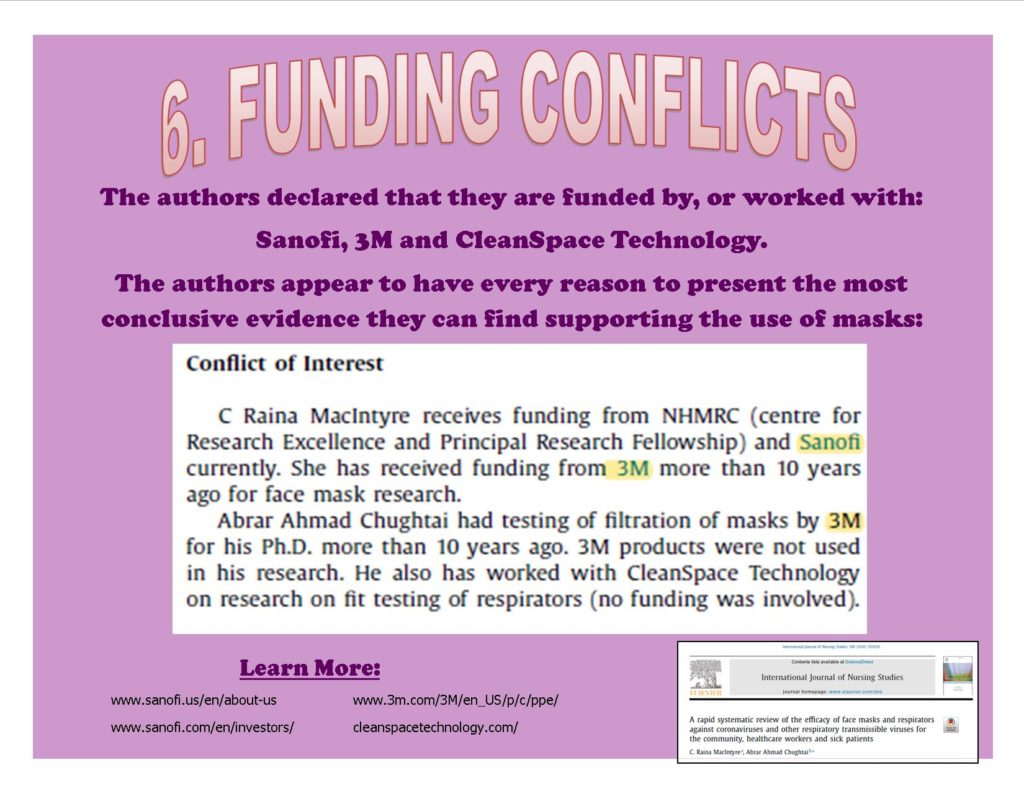
Let’s try going through the steps with this example: A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients
This study reviews research focused on the use of masks in healthcare and community settings. Read the study for yourself and see if it’s findings support the use of masks in community settings.
Below is a slideshow which takes us through the steps, but you are sure to find more if you read the study yourself!
Vermont Towns SPEAK UP!
In November, 2021, the Vermont Legislature decided to give town Selectboards the power to mandate masks. Town by town, Vermonters have been weighing in on the idea of town-wide mask mandates.
Towns have overwhelmingly decided against mask mandates: 3 to 1.
In essence, Vermont has now held a public referendum on the issue of masks, and testimony given at the public meetings makes it clear that people are suffering harm, and are well-informed of the science. Meanwhile, those who support the use of masks could only refer to certain “expert” opinions, and had no evidence to support these opinions.
For example, a letter signed by 12 medical professionals in Danville contained a “message in a bottle.” The letter was written to the Danville Selectboard members in order to encourage the use of masks. However, the only study it references as evidence actually describes the known harms caused by masks:
Read the study referenced in the poster above: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7646657/
To hear testimony from Vermonters during the town Mask Mandate hearings, see the Videos/Interviews with VMS Author page on this website. (Tab at the top of the page.)
Information about the harms of masks is constantly being censored. To hear what is being said, but not televised, check out my list of Second Opinions: https://amyvt.com/wp-content/uploads/2021/03/Second-Opinions.Valid-Viewpoints.pdf
We need to begin having a fair discussion about this important topic.
To contact this website author with questions or evidence to share: vtmasksurvey@mail.com